Editor’s note: This Science Based Medicine blog post is another collaborative effort between Grant Ritchey and Clay Jones. Not only have they previously co-authored an SBM post on fluoride, their partnership has recently expanded into other areas of science journalism. Since the departure of Dr. Jason Luchtefeld as co-host of The Prism Podcast, Clay has joined Grant as the new co-host. To this end, Clay and Grant have added a Science Based Medicine segment to each podcast episode, in which recent SBM blog posts are reviewed and discussed with the authors themselves. Check them out on iTunes or your favorite podcatcher.
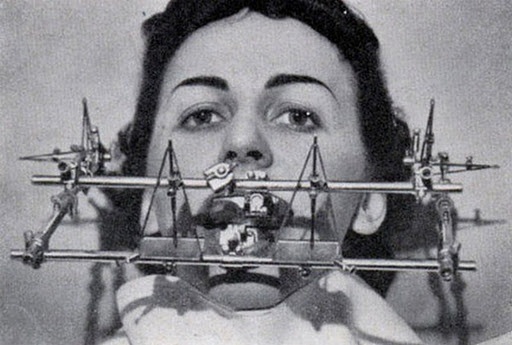
“We’ll remove that headgear when your tics improve.”
One of our primary goals is to promote the concept of scientific skepticism and the importance of prior plausibility when interpreting new research. On the pages of this website, and in extracurricular activities like our various podcasts and personal blogs, we often call upon these two load-bearing pillars of science-based medicine when investigating implausible and unproven claims championed by well-meaning true believers and outright charlatans. What our collective experience has revealed time and time again is that both will often hope that a gullible public will put their trust in a warped version of science, while relying on emotional responses to anecdotes and testimonials.
In our post today, we will walk readers through our investigation of thus far unproven claims involving the treatment of a complex neurological disorder, Tourette syndrome (TS), with a fitted dental appliance aimed at improving the alignment of a patient’s jaw. From the perspective of a dentist (Grant) and a pediatrician (Clay), there aren’t any obvious connections between the jaw and this childhood-onset neuropsychiatric disorder, but proponents believe that there is one and that these appliances can significantly reduce the severity of symptoms. Although impossible to enter into an investigation such as this completely free of emotion or bias, we truly attempted to keep an open mind throughout the process.
First up, a disclaimer:
Clay was diagnosed with Tourette syndrome when he was 7 years old. As both a pediatrician who has now cared for a number of patients with TS and someone who has personally experienced many of the negative physical and social sequelae associated with the condition, this is a topic that Clay takes rather personally. Although his symptoms are now on the milder end of the severity spectrum, and are far from debilitating, they do often serve as a source of frustration in his day-to-day life. The thought of children with Tourette syndrome being taken advantage makes him angrier than that time somebody switched out his regular coffee for Colombian decaffeinated crystals.
Without hesitation, we would love for there to be another effective treatment option for Tourette syndrome in our armamentarium, especially one that would be essentially risk free and relatively inexpensive. Again, as scientific skeptics we are open to new evidence as it emerges. But before we get to the claim and the research being used to back it up, we will give a primer on the scientific consensus on TS so that readers can better assess for themselves the prior plausibility of this proposed treatment.
What is Tourette syndrome?
Tourette syndrome is a complex and historically misunderstood neurological disorder resulting in an astonishing variety of involuntary but transiently-suppressible movements and vocalizations known as tics. TS is also frequently associated with numerous comorbid conditions such as attention-deficit/hyperactivity disorder (ADHD) and obsessive-compulsive disorder (OCD) – 60% and 30% respectively. Over the years, our understanding of the incidence of TS has changed considerably. No longer thought to be rare, a recent meta-analysis and systematic review of prior prevalence studies found that TS affects at least 1 out of every 200 children, with boys more likely to be diagnosed than girls by a ratio of 4 to 1.
If that prevalence estimate feels high to you, there is good reason. The severity of TS symptoms is highly variable, ranging from barely noticeable to completely debilitating. Symptoms aren’t even consistent in an individual patient, with significant waxing and waning over the course of a patient’s life being the norm, and shorter periods of acute changes related to stress, distraction, and temporary conscious control. You have almost certainly been around folks with TS and had no idea.
Many people, when conjuring up an image of the typical TS patient, are likely influenced by the numerous inaccurate portrayals in movies and on television. Or their concept of the condition has been biased by countless jokes made at the expense of patients with the disorder, which is often used as a punch line whenever something socially inappropriate occurs. In fact, the only reasonable portrayals we have seen are the movies The Tic Code and Front of the Class, and the documentary I have Tourette’s, But Tourette’s Doesn’t Have Me. Sadly, the lazy jokes (we are looking at you Jimmy Fallon) and terrible film portrayals are considerably more prevalent, and they have contributed to a general public ignorance that increases the risk of misdiagnosis, delayed diagnosis, and bullying.
What are tics?
The most recognizable feature of TS is the tic. These are purposeless movements or noises that occur suddenly, often in bursts, and may seem random to witnesses. But appearances can be deceiving. Although generally considered involuntary, and they can at times take patients by surprise, tics are usually preceded by an intense urge that can usually be suppressed voluntarily with varying degrees of mental effort, a phenomenon that is universally described by patients with the condition. Think of the tic as scratching a sort of internal itch, an itch that might feel good to scratch at times but is a near-constant source of frustration and annoyance for many patients with TS.
Tics can be simple movements, such as eye blinking, grimacing, or jerking of the head or arm, or surprisingly complex behaviors involving multiple muscle groups, such as an unusual gait or a patterned movement of the fingers. They can even be meaningful, ritualistic, or obscene in some cases. Tics can be violent or subtle, easy to conceal or extremely disruptive depending on the setting. Motor tics, in particular severe jerking of the head, can even cause injuries such as cervical disk herniation and dissection of a cervical artery in rare cases.
Vocalizations have a similar categorization into simple and complex vocal tics. Grunting, throat clearing, and sniffing are extremely common, but vocal tics can manifest as words and phrases as well. The most widely known and also misunderstood vocal phenomena associated with TS, thanks to the aforementioned misleading characterizations, is that of coprolalia.
Coprolalia (please read this one) involves the involuntary utterance of obscene words or phrases, although some patients merely think the words or mutter them under their breath. It is believed to occur in 10-40% of patients. But because many patients with mild TS aren’t diagnosed, and studies historically have tended to select for the more severe cases, the prevalence of coprolalia is likely exaggerated.
Coprolalia is fascinating and is a good example of the interplay between TS and OCD, which will make more sense after we’ve discussed the involved neuroanatomy. It is also extremely distressing to patients and often results in extreme social isolation and a severely affected quality of life. It isn’t funny. If you didn’t click on that last link, here it is again.
Here is a list of common tics seen in patients with TS that is not to be used as part of a twisted drinking game at next year’s NECSS.
Although which tics that an individual with TS develops are essentially random, most patients have specific tics that are consistently present. These tics may wax and wane in severity over the years, but they tend to always be there as long as a patient is having tics. Because of this, and the fact that tics in novel anatomic locations do also develop, there is the appearance of a migrating tic pattern. Thankfully in most patients, overall tic severity tends to decrease substantially after adolescence and many adult patients consider themselves to be tic free.
But, and this is very important in the context of evaluating claims of success in treating the condition, more than half of adults who consider themselves to be tic free were not when video evidence was reviewed by a blinded observer. This study didn’t even involve patients undergoing a novel therapy. It was just random adults with a history of TS. There is no reason to assume that adolescents or younger children would be any more accurate.
TS symptom severity is not always easy to assess over any duration of time. When it comes to long term changes, unless someone is secretly videotaping a patient and then carefully counting up tics, it comes down to an easily-biased personal or caregiver assessment. Complicating matters is the waxing and waning nature over long periods of time. If a treatment is started just at the start of what would have been a lull in a patient’s tics, or immediately after an unusually severe period, it can appear to work.
Evaluations of tic frequency for short periods of time, such as immediately before and after an intervention or during an office visit to film a testimonial for your chiropractor, is also prone to error. Severity can increase or decrease significantly from baseline during brief encounters due to stress, relaxation, or suppression, which can be conscious (job interview) or unconscious (increased focus on something else or not wanting to disappoint your parent/chiropractor). TS has historically been difficult to diagnose because kids are notorious for suppressing tics in the doctor’s office. Now caregivers can just use their smartphone to capture tics without the child knowing.
What causes Tourette syndrome?
Although the exact underlying pathophysiology of TS is not completely clear, it is widely considered to be the result of a complex combination of social and environmental factors with genetic abnormalities that alter the structure and function of specific areas of the brain. Although there are some gaps and shadows within which pseudoscientific claims can gather, scientific study has revealed more than what some believers would have us believe.
Environmental and psychosocial variables, while not causative, can play a huge role in the severity of tics in many patients. Stress and anxiety, such as being emotionally upset during an argument or having problems adjusting to a new school, are well known factors in tic exacerbations, as is stress from an acute or chronic illness. From an environmental perspective, there have been links to caffeine and other stimulants as well as maternal smoking, low birth weight, and many more.
There is clearly a genetic component to TS. When thoroughly investigated, TS symptoms can be found in the family history of the vast majority of patients. And the children of a parent with TS have a more than 50% chance of developing tics, with roughly a quarter of them meeting diagnostic criteria for TS. The risk is even higher when TS runs on both sides of the family.
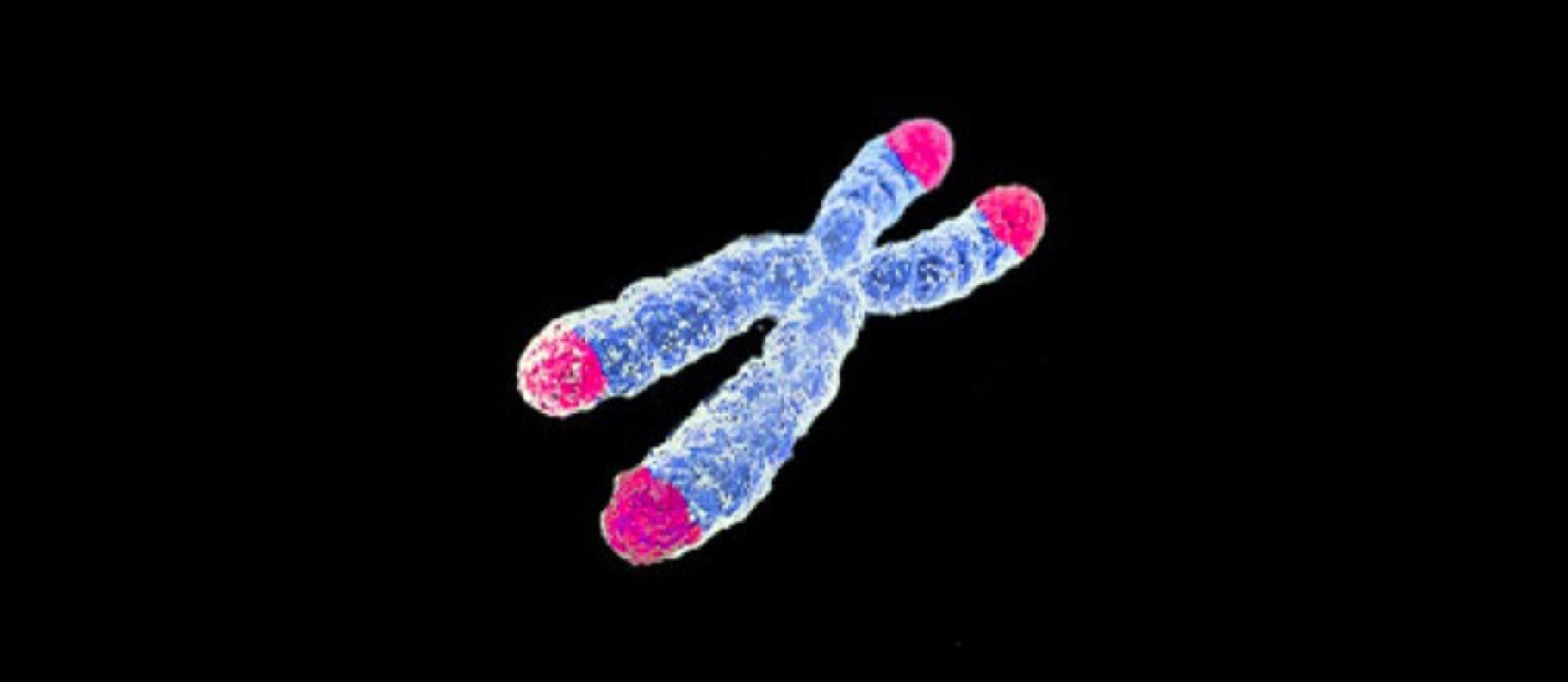
The exact genetic abnormality, or more likely the additive abnormalities in multiple areas of the genome, isn’t known. Over the past several years, multiple candidate regions have been identified, the most interesting so far being a mutation in the SLITRK1 gene on chromosome 13q31.1. This particular gene, which would only explain a small percentage of cases, plays a role in the function of areas in the brain long believed to play a key role in TS, specifically the mesolimbic and frontostriatal pathways.
These areas of the brain, particularly the thalamus, basal ganglia, and frontal cortex, involve connections between movement and behavior and are also implicated in OCD and ADHD, which makes sense considering how frequently these conditions coexist in a TS patient. Although multiple neurotransmitters play a role in the function of these circuits, it is widely believed that a problem with dopamine is the culprit when it comes to TS. Whether there are excess amounts of dopamine or hypersensitive dopamine receptors is unclear.
Gross examination and standard imaging of the brains of TS patients haven’t been helpful, but advanced modalities have increasingly revealed structural and metabolic abnormalities. Patients with TS tend to have decreased volume in the left frontal lobe and overall reduced depth and thickness of gray matter. Metabolic studies have shown increased glucose utilization in the premotor cortex and cerebellum with reduced striatal and orbitofrontal activity. These areas of the brain play a role in the planning and control of movement, as well as in our dopamine-saturated internal reward system, perhaps explaining the urge to tic, the ability to have some temporary control over tics, and the pleasurable feeling when a tic is performed.
Caudate nucleus volume loss as seen on high-resolution MRI is probably the best evidence we have of a clear abnormality in a specific region of the brain. Although still preliminary, it appears that the smaller the caudate volume, the more severe the symptoms of TS and the more likely there will be associated OCD. The caudate nucleus, the activity of which is strongly linked to dopamine activity, plays a key role in the control of movement and in the development of Parkinson’s disease, but also executive function. It’s kind of a big deal.
Of course not knowing all the genetic underpinnings and the exact neuroanatomical abnormalities is not the equivalent of them being unknowable. Clay even recently took part in research at Massachusetts General Hospital, where cutting edge genome-wide association studies are underway. And investigation using advanced neuroimaging techniques is ongoing in numerous research facilities. Stay tuned.
How is Tourette syndrome treated?
Thankfully only a small percentage of those diagnosed with TS will actually require any form of pharmaceutical treatment, although some can’t make it through a day without it. For most, education (patient, family, teacher, employer, etc), reassurance, and monitoring for impairment are all that is necessary. Impairment can come in the form of social upheaval, school or work problems, difficulty with daily living activities, subjective discomfort, pain, or injury.
Patients who present with severe symptoms typically require a prescription as part of their management. For milder cases, although most patients would probably benefit to some degree, only behavioral therapy may be recommended. This typically comes in the form of cognitive behavioral therapy or habit reversal therapy. This can be very helpful alone and as an adjunct to drug therapy, which makes sense considering the significant role that stress plays in overall symptom severity, but it takes a lot of time and effort. And availability is unfortunately limited for many patients.
Historically, the drugs used for TS have blocked dopamine receptors. This is yet another clue to the role of dopamine in the underlying pathophysiology of the condition. The most well-known of these is probably haloperidol, which is better known as an antipsychotic medication but it has a wide variety of uses. Tetrabenazine, a drug that reversibly lowers dopamine levels in the brain, is becoming the treatment of choice because it is equally effective and considerably safer. Most patients experience a 60-80% decrease in tics.
There are other pharmaceutical options, particularly alpha-2 adrenergic stimulators like clonidine which have a general calming effect on the brain. These tend to be less effective but may be better tolerated in some patients and are safer than traditional antipsychotic drugs like haloperidol. In patients with significant behavioral symptoms, like ADHD, these medications play a larger role.
In general, when comorbid conditions are present the drug choice is determined by the aspect of TS that is causing the most problems. Treating severe ADHD with clonidine or even a stimulant medication may actually lead to significant improvement in tics that were exacerbated by the stress caused by the behavioral problems. Treating OCD with behavioral therapy or a selective serotonin reuptake inhibitor may reduce tic severity. Treating problem tics may improve ADHD/OCD symptoms. There is nuance to the management.
Enter the dentists
As was mentioned, TS can have profound physical and psychosocial effects on the individual, as well as creating worry and stress among family members. It is therefore not surprising that some patients or caregivers will go to great lengths to try to obtain relief, either because conventional options aren’t as effective as desired or because they are hesitant to try them. Promises of safe and effective treatments that don’t involve medications may be believed uncritically out of desperation and vain hope.
Parents in particular are a vulnerable population. What parent wouldn’t go to any effort to obtain relief for their suffering child? Sadly, this desperation creates fertile ground in which well-meaning as well as unscrupulous purveyors of alternative medicine plant their unique ideas for management of this condition. Questionable non-scientific treatments for Tourette syndrome run the entire woo gamut – from chiropractic to acupuncture to supplements.
We live in an amazing era of modern dentistry. Gone are the days of Marathon Man and Little Shop of Horror appointments; thanks to measures such as fluoride, sealants, and beautifully lifelike restorations, people can enjoy a level of dental health and aesthetics never before experienced. Relatively recent development such as dental implants allow dentists to restore comfort, function, and appearance in formerly hopeless situations.
One of the most versatile tools in the dentist’s arsenal is the use of acrylic dental appliances to treat or manage a plethora of dental issues. From bite splints to mitigate the effects of bruxism (tooth grinding), to appliances to manage obstructive sleep apnea, to functional orthodontic appliances and retainers – the list goes on and on. There’s almost no problem a patient could have that a hunk of acrylic can’t make better.
There have been a handful of dentists who have claimed that they can alleviate the symptoms of Tourette syndrome and other movement disorders by use of a dental appliance, similar in many ways to the ones used to treat temporomandibular disorders (TMD). Drs. Anthony Sims and Brendan Stack have been at the forefront of this area of study for several years, and have published papers on this subject. Granted, these papers are preliminary and published in low impact journals, but these respected and well-intentioned dentists are trying to support their treatments with a scientific underpinning. Sadly, the science isn’t there yet as we shall see. There is almost nothing in the literature about dental appliances and the management of Tourette syndrome on PubMed or in the Evidence Based Dentistry website at the American Dental Association.
We will take a brief look at two of Dr. Sims’ and Stack’s papers to set the stage for the rest of our discussion. The first is a pilot study of their dental appliance, which has the distinguished if not Spanish Inquisitionish sounding name of Neurocranial Vertical Distractor (NCVD). This paper, published in the Journal of Craniomandibular Practice, outlines the current science on Tourette syndrome. After describing what “mainstream medicine” believes about it, the authors then take a detour, stating:
Many movement disorders are believed to be disjunctions within the thalamus-cortex-substantia nigra connections. However, the authors believe the neuroanatomy of this movement disorder does not rise to the high level of these connections, but is a reflexive disorder that occurs at the spinal cord level within the spinal trigeminal nucleus, specifically the subnucleus caudalis.
They base this hypothesis on their observation that many of the habitual movements of people with TS occur due to reflexive tics of muscles innervated by the trigeminal nerve, or Cranial Nerve V. They then extrapolate this observation to infer that the symptoms of TS and other movement disorders are a function of an “overstimulation” of the neural impulses carried by the trigeminal nerve to the brain due to dysfunction within the temporomandibular (jaw) joint. By treating movement disorders as a TMJ disorder, they reason that a multitude of symptoms can be reduced or eliminated. The NCVD ostensibly reduces this excess neural “noise” by decompressing or distracting the mandibular condyle (head or ball of the lower jaw) from the glenoid fossa (socket), decreasing pressure on the sensitive tissues innervated by the auriculotemporal nerve, a division of the trigeminal nerve. Looking at the device (refer to page 7 in the above article), one can see the thick areas of acrylic on the biting surfaces of the appliance. It is this thickness between the wearer’s teeth, which is determined by the dentist on an individualized basis, which keeps the mandible down and forward in the therapeutic position. The pilot study concludes with a case report of five cases successfully treated with the NCVD.
The other article is an expansion of the first, going more deeply into the proposed neurology and biochemical mechanisms involved in how a dental appliance would reduce or eliminate the symptoms of TS. In the journal Medical Hypotheses, they state:
We hypothesize that the majority of T.S. patients with their various comorbid disorders are due to malposition of the mandible to the patient’s cranial base, resulting in constant stimulation to the trigeminal system that is below the threshold of noxious pain input.
This is indeed an interesting hypothesis, and if true could give hope and relief to millions of people with Tourette syndrome worldwide. No drugs, no surgery – it sounds too good to be true. Adding to the emotional impact of Dr. Sims’ and Stack’s theories, there are many compelling YouTube videos (examples here and here) that purport to show dramatic, almost miraculous responses to the NCVD. These articles are hypothesis-generating and deserve the opportunity to be vetted through rigorous scientific studies and well-controlled trials.
More recently, a new player has entered the game, and this player has barged into the arena boldly and loudly. New York sports radio host Craig Carton, who has Tourette syndrome, has committed $340,000 from his foundation, TicTocStop, to fund device research. Partnering with the University of Tennessee College of Dentistry, Carton wants to help sponsor research in this area. While on the surface this seems an extremely generous and worthwhile endeavor and we certainly don’t want to disparage his intent or actions, there’s a taint about it that we want to address.
First and foremost, anyone who holds a science-based worldview will accept (and hopefully agree) that before a medical product or technique is brought to the public, it must undergo the necessary testing to ensure that it is safe, effective, and better than what is currently available in some way. Basic science research, lab research, and clinical trials are often needed to provide this level of confidence. In this case, however, there is an advertising and branding blitz ahead of the research, and it seems that they are trumpeting the yet-to-be-done research as a marketing tool to infuse some pre-emptive legitimacy to the project.
Their website is heavy on the glitz and light on the science. Their straight to TV campaign on The Doctors show was pure Barnum and Bailey. On it, Mr. Carton stated “…for a hundred years, there’s been not a single advancement in research…” followed by the heart of the message: “We’re selling hope. That’s all we’re selling.”
As responsible health care professionals, that concerns us. We’re neither neurologists nor TS specialists, but we’re pretty sure that there has been at least one scientific advancement in Tourette syndrome research since The Great War. And hope is the only thing they are selling? This appliance will most likely not be covered by medical or dental insurance, so this “hope” that they are selling without proof of efficacy could cost desperate patients and parents thousands of dollars in out-of-pocket expenses.
Grant emailed Timothy L. Hottel, D.D.S., M.S., M.B.A., Dean of the University of Tennessee College of Dentistry and Principal Investigator (PI) of the TicTocStop research project, asking for more information, including study design. Grant informed him that he and Clay were working on an SBM article and wanted his input in order to be “objective and accurate.” His response was as follows:
Dr. Ritchey
Thank you for your interest in our research project. Although I am the PI for this project, it is being completed for TicTocStop. Therefore, I am bound by contract not to release any information on this project….
He then forwarded Grant’s email to Dr. William Balanoff, the medical director for the TicTocStop company (and the guy in the lab coat on the TV show clip), who replied:
Dear Dr. Ritchey,
I read with interest your email to Dr. Hottel. You bring up many good points that need to be addresses [sic] by science in general and dentistry/medicine in particular. Like most research (this included)…it is a journey with no end; only milestones.
As we learn, we will share the information with the world. That is what science does. At this point it is too early to know anything conclusive. I have your contact information and will reach out to you when the research and results achieve some conclusion. I appreciate your zeal to report and comment on this very important study. Let’s stay in touch.
We appreciated both of them responding in a timely and courteous manner; however, we were not given anything of substance. Dr. Balanoff did not respond to a follow up email requesting more information about the proposed study. We understand that in the commercial world, there can be proprietary information that they might not want to reveal – appliance design, materials, what lab they certify to make the appliance, etc. However, in the interest of transparency, why would they not share the experimental details? Are they afraid they will be called out for poor design? Improper blinding? Small sample size?
If the results don’t support their commercial venture, will they move the goalposts or file drawer the study? I guess we won’t know until and unless they publish their data. As staunch supporters of the AllTrials Initiative, we believe that clinical trials should be registered and monitored so that all results are published, not just the ones which have results that benefit the researchers or vested interests. To this end, we challenge Dr. Hottel, Dr. Balanoff, and the TicTocStop research team to register with the AllTrials campaign to ensure that the research is transparent and provides maximum benefit to the scientific community and society at large.
We wish we didn’t have to take such a pessimistic look at this situation, but so far we have seen very little that would lead us to think otherwise. No one is rooting for their success more than we are (especially Clay), but when a venture has all the trappings of a commercial venture, we must raise our eyebrows. Grant has seen this model before in the dental world with a different sort of appliance, and it didn’t end well.
Pulling out his crystal ball, he cynically sees the scenario playing out something like this: TicTocStop will market the hell out of their appliance directly to the consumer via Tourette syndrome support groups, online communities, parenting magazines, and so on. They will be on news shows and all over the web. They want TS patients to ask their physicians and dentists for them, creating a huge demand from the “bottom up”.
They will want to generate some buzz. Moreover, they will mount a huge marketing campaign directly to dentists, informing them of this huge opportunity to help people (and make a lot of money in the process), charging a hefty fee for them to attend TicTocStop’s continuing education courses where they will learn how to properly evaluate and treat the TS patient with their proprietary appliance. Dentists who attend their course will have the privilege of having their name listed on the TicTocStop website as a referral source to drive new patients to their offices, and will have permission to use the TicTocStop logo and promotional materials.
Labs will pay a lot of money to become a TicTocStop “certified lab”, granting them an exclusive license to fabricate the TicTocStop appliance, which will be expensive to fabricate. Meanwhile, we may or may not ever know the results of the study, depending on how well it was done and what they found (or if they accepted our challenge to register with AllTrials). If the study was well designed and carried out properly, taking into account the difficulties in assessing TS symptoms we described above, we predict that the results will be negative, which would be decidedly inconvenient for them. If the study isn’t very robust or well executed, then it will probably be positive, which they will parade around proudly.
Will conflicts of interest be disclosed? Please forgive our pessimism, and we certainly don’t want to impugn the good people at the University of Tennessee or at TicTocStop. Despite our glum prognostication, we would like to go on record to state that we have no doubt that all of the participants and investigators involved in this project sincerely want to help those with Tourette syndrome. And we also recognize that in this age of tight funding, the money for research has to come from somewhere, so we don’t fault them for their fundraising and commercial efforts.
But when profiting from such a situation gets too far ahead of the science and perhaps even trumps it as a priority, it raises our concern and ire. Money has the potential to generate a lot of bias and cognitive blindness, something we call The Daddy Warbucks Fallacy. We earnestly hope that we are proven wrong on all counts.
Parting thoughts
In our opinion, based on the consensus understanding of its underlying pathophysiology there are some major plausibility concerns with the hypothesis that disorders of the temporomandibular joint play a role in the development of TS symptoms. The number of assumptions required certainly violates Occam’s razor, and it raises many questions:
- Tics are present in virtually all muscle groups, not just the muscles of biting and chewing. Why assume that the trigeminal nerve is the culprit? Many assumptions must be made to connect the trigeminal nerve to blinking, let alone shoulder shrugging and coprolalia that don’t make any sense neurologically.
- How does trigeminal “overstimulation” lead to the changes in the brain neuroanatomy seen with advanced imaging, or are those a coincidence? To our knowledge, there are no other medical conditions with a similar pathophysiology. There already is a condition involving chronic injury of the trigeminal nerve called trigeminal neuralgia, however, and it causes severe facial pain but no other neurologic symptoms.
- Assuming “overstimulation” of the trigeminal nerve can result in neurological symptoms, why does it selectively cause tics, ADHD, and OCD and not seizures, schizophrenia, personality changes, or some other neurologic problem? What explains the urge to tic?
- Why is there a clear genetic pattern to TS? TMD does not run in families to anywhere near that degree.
- How does TMD as a factor explain the waxing and waning course of TS and the fact that most patients have significant improvement after puberty? Does malposition of the jaw improve after puberty and as patients age?
In summary, while we can’t yet discount the possibility that a dental appliance, be it a Neurocranial Vertical Distractor or a TicTocStop appliance, can lessen or eliminate the tics that Tourette syndrome patients have, we can conclude that the biological plausibility for such a device is very low. What we know about TS doesn’t jibe with dental hypotheses. YouTube videos and testimonials, as impressive as they may seem, are insufficient because the natural course of TS and the role stress/placebo plays can make absolutely any intervention (and in particular for neurological problems) seem to work in the short run. And the literature on the subject has essentially been a monopoly by two dentists who treat Tourette patients and is scant and of low quality.
Ultimately, readers will need to decide if this is an extraordinary claim or if repositioning of the jaw in an effort to reduce the neuromuscular manifestations of this complex disorder is in line with our basic scientific understanding of neuroanatomy and the consensus pathophysiology of TS. Once a sense of the prior plausibility is determined, the degree of evidence required to make a causal claim can be decided. Then a provisional conclusion can be made that may or may not change if new data is actually published.
At this point, we would caution anyone who has TS, or is the caregiver of someone with the condition, to be wary of these claims until the science can better support it.