In a person with prediabetes, blood sugar levels are raised but not yet to within the ranges of diabetes.
Although not a lot is known about how many people have prediabetes, one study found that the condition affects 1 in 3 adults in the UK. According to the Centers for Disease Control and Prevention (CDC), the same prediabetes rates affect Americans.
Without treatment, an estimated 15-30 percent of those with prediabetes go on to develop type 2 diabetes 5 years after diagnosis.
Many prediabetes prevention plans revolve around two key lifestyle factors – a healthy diet and regular exercise.
The results of the Diabetes Prevention Program, run in the United States since 2001, suggest that losing an average of 15 pounds in the first year of a prediabetes prevention plan reduces the risk of developing type 2 diabetes by 58 percent over 3 years.
Researchers from John Hopkins University also found that a combination of diet and exercise help. When both were used to achieve a total body weight loss of 10 percent or more in the first year of a prevention plan, the risk of type 2 diabetes fell by 85 percent within 3 years.
Contents of this article:
The prediabetes diet
There are a few different ways to plan a prediabetes diet. The Mayo Clinic suggests diets filled with low-fat, low-calorie, high-fiber, foods. That means lots of fruits, vegetables, whole grains, lean meats and protein-packed legumes. It also means avoiding artificial sugars, added sugars, and fats.
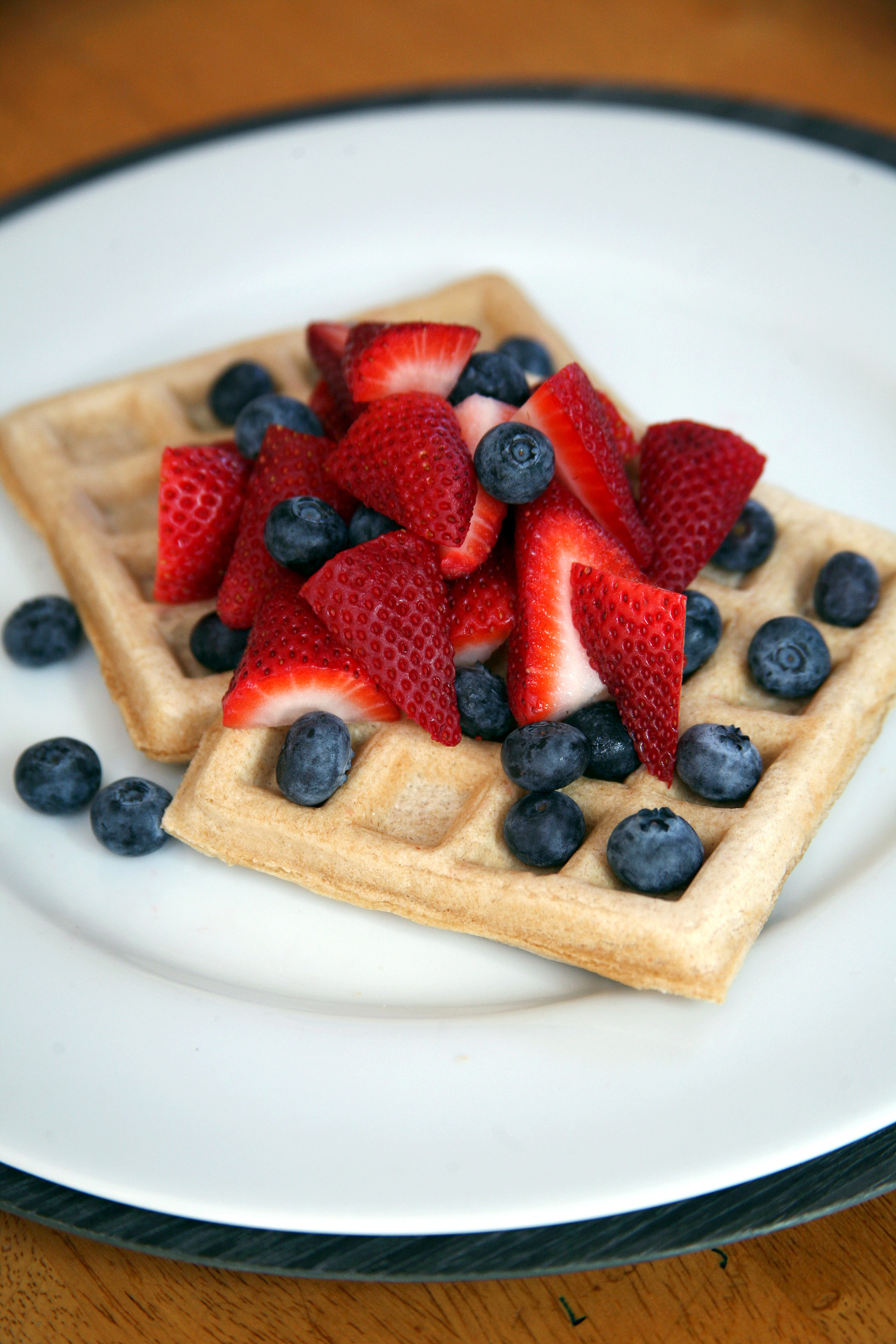
Fruits and vegetables are recommended for people with prediabetes.
To help guide meal plans, the Glycemic Index (GI) is a useful tool. It ranks foods by the rate at which they affect blood sugar levels. Some carbohydrates are digested slowly, gradually releasing sugar into the bloodstream. Others are processed quickly, causing a quick rise in blood sugar levels.
Because prediabetes prevention plans aim to steady blood sugar levels, low and moderate GI foods are the foundation of most prediabetes diets plans.
Foods with a GI value of 55 or less raise blood sugar levels slowly, while those with a GI value of 70 or above raise blood sugar levels much faster. Foods with GI values between 56 and 69 are classified as having a medium GI value, altering blood sugar levels at a moderate rate.
It’s not easy to tell a food’s GI value simply by looking at it, but there are some tips to follow:
- Foods high in refined sugars or fats usually have a higher GI value than low-fat, natural sugar-containing foods
- Whole wheats, cereals, and grains all tend to have lower GI values than traditional white breads, cereals, and rices
- Sweet potatoes, most vegetables, whole fruit, and legumes have lower GI values than white starchy vegetables like potatoes
- As most fruits and vegetables ripen, their GI value becomes higher
- Low fat or reduced fat options have far lower GI values than creams and whole milk
- Pastas are typically low GI foods because of the way their starches are bound
- Vegetable noodles like udon and vermicelli are also great low GI options
- Parboiled rice, basmati, and brown rice all have lower GI values than short-grain or jasmine rice
- Most species of fish have far lower GI values than pork, poultry, and beef
- Homemade oatmeal or stone-cut oats have a lower GI count than packaged oatmeal
For a better idea of how specific foods rank, Harvard Medical School hosts a list including the GI values of 100 common foods.
There is also several tools available online. These include low GI shopping lists, recipes, health meal e-newsletters, diet and exercise routines, and trackers. Some foods even carry a GI symbol.
Prediabetes risk factors
Just like diabetes, prediabetes is a metabolic condition, so most things that interfere with the body’s ability to metabolize, absorb, or store energy can influence the condition.
Blood sugar levels can be raised because of insufficient insulin production, impaired insulin expression, or because cells don’t respond properly to insulin.
Age, weight, and physical activity have all been shown to play a major role in prediabetes. Those most at risk are generally above the age of 40, inactive, and overweight or obese.
Ethnicity and culture may affect the risk of prediabetes. Countries and cultures with higher rates of diabetes also have higher rates of prediabetes. Pacific Islanders and South Asians, as well as those of African, Caribbean, Asian or African American, Hispanic, and Latino descent are all at higher risk of developing the disease.
Other risk factors include:
- Having a direct relative with diabetes
- High blood pressure
- High circulating triglycerides levels
- Low levels of “good” cholesterol, known as high-density lipoprotein (HDL)
- Excess belly fat
- Other specific conditions, such as polycystic ovary syndrome (PCOS), gestational diabetes, and low testosterone in men
- Heart disease
Prediabetes warning signs
The symptoms of prediabetes are often hard to spot. At times, there are no symptoms at all.
Increased thirst and urination are traditional signs of the disease. Constant raised blood sugar levels can also cause extreme tiredness, make it hard to concentrate, and lead to unexpected weight changes.
A darkening of the skin called acanthosis nigricans can also occur on various parts of the body, such as the neck, elbows, knuckles, and knees. Everyday wounds can also take more time to heal than normal.
Prediabetes prevention plans
Managing prediabetes often takes the right combination of diet, exercise, and weight loss.
An exercise plan is one way in which people can manage prediabetes.
Prevention plans focus on lowering and steadying blood sugar levels. This is achieved with activities that use up excess blood sugar and foods that promote the slow, gradual release of sugar into the bloodstream.
Exercise and Sports Science Australia recommend that people with prediabetes get 210 minutes of moderate-intensity exercise or 125 minutes of rigorous exercise each week. The American Diabetes Association (ADA) recommend 30 minutes of any form of activity at least five times per week, preferably every day.
Activities from running to brisk walking, strength training, and flexibility work all count toward this goal.
Exercise can do a lot to work out extra sugar in the system, burning up energy otherwise turned into fat for storage.
There is plenty of new research adding to the list of preventive prediabetes measures. A recent study in the American Journal of Respiratory and Critical Care Medicine found that the use of continuous positive airway pressure (CPAP) machines lowered blood sugar levels in people with sleep apnea. Therefore, if you have an undiagnosed sleep disorder and start treatment, it may have a significant impact on your prediabetes.
However, all sugar in the blood comes from food. As a result, diet is a crucial part of any prediabetes management plan.
Other diet tips for prediabetes
The American Diabetes Association (ADA) claims that those who have success following prediabetes diets have a few things in common. Aside from simply cutting back on calories and fats, routine is crucial to keeping blood sugar levels even.
Those with prediabetes should avoid events that cause significant changes in blood sugar levels like fasting. Eating properly portioned meals regularly throughout the day is key to this goal. It is also important to make sure meals are balanced, with each containing a source of protein, fat, and carbohydrates.
Groups like the Canadian Diabetes Association also support the use of more traditional weight management techniques in prediabetes management plans, such as the plate method and carbohydrate counting.
Eating out can be hard for anyone trying to stick to a diet. General tips include splitting meals, favoring starters, and reviewing the restaurant’s menu ahead of time.
Though some people will require the use of prediabetes medication alongside diet and exercise adjustments, recent studies have found physicians rarely rely on drugs.
A study in the Annals of Internal Medicine found that American physicians prescribed the drug metformin in less than 4 percent of prediabetes cases.
Research from the University of Leicester in the UK suggests that dietary changes, coupled with increasing exercise, has far more of a preventive impact than medication alone.