A new study shows that 42 really is the answer to life, the universe, and everything. OK, not really, but it does show that 42% of healthy brain activity is the minimum threshold for consciousness.
Disorders of consciousness, also referred to as coma when severe enough, can be a difficult situation to assess sufficiently to make reliable predictions about outcome. Part of the problem is that once someone is not able to maintain consciousness, we lose much of the neurological exam, and therefore it becomes more difficult to assess brain function other than to say that they are not conscious.
Types of coma
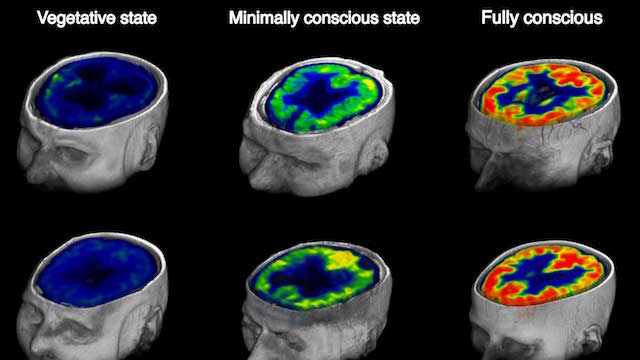
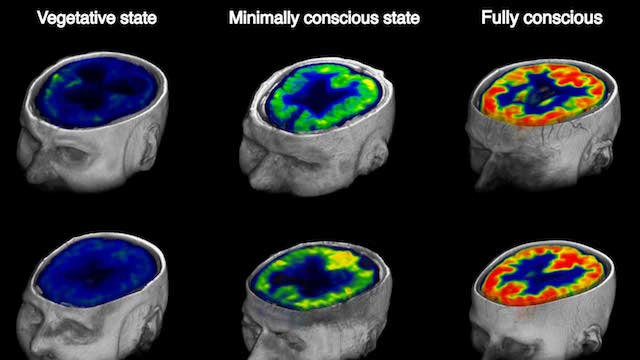
Two types of coma in particular are of interest: the persistent vegetative state, also called unresponsive wakefulness syndrome (UWS), and the minimally conscious state (MCS). Both are severe impairments of consciousness. In UWS, by definition, the patient may have sleep-wake cycles, open their eye, have roving eye movements, and grimace, but they do not have any interaction with their environment. They do not respond to voice, look at faces, or move in response to stimuli.
MCS is similar, except that patients give minimal signs of consciousness. They may attend to a face, or move in response to stimuli, but cannot communicate or participate in their care. There is a continuum, of course, from the MCS to a fully conscious state.
Sometimes it can be difficult to distinguish MCS from UWS. In a previous study, 41% of patients who were diagnosed as being in a UWS by standard neurological exam were actually in a MCS when a more thorough neurological exam was conducted.
Later research found that using fMRI scans (which measure blood flow) or quantitative EEGs (which measure electrical activity) were even more sensitive at distinguishing MCS from UWS. However, a 2014 study showed that a PET scan, which measures tissue metabolism, was even better at predicting who had signs of consciousness and also who might recover function a year later.
Of note, this research tends to show that patients who have impaired consciousness due to diffuse anoxic ischemic damage (lack of blood flow to the brain) had poor function and poor prognosis. They tended to really be UWS and not recover. Meanwhile, patients in a coma due to trauma were more variable. Some had more function and more potential to recover. This makes sense as trauma patients may look worse due to focal damage but still have some hidden brain function, while anoxic ischemic patients have damaged their entire brain.
The new PET study
With this background comes the new study, which includes many of the same researchers as the studies I mention above. They looked at PET scanning, because that showed the most potential in previous research, and also looked at trauma patients, because they also showed the most potential in previous research. They examined 131 head trauma patients using [18F]-fluorodeoxyglucose (FDG) PET scanning, and then followed them for a year as they recovered. They found several interesting things.
First, by quantifying overall brain metabolic activity they found that the minimal activity necessary to produce a conscious state was 42% of normal activity (determined by examining healthy controls). Simply put, the brain has to be able to produce a certain minimal amount of activity in order for conscious wakefulness to emerge.
Further, there does not seem to be any part of the brain that was essential for consciousness. There is no “seat of consciousness.” Consciousness is a whole-brain phenomenon, and all parts of the brain contribute their bit to consciousness. This fits with the current science of consciousness, which has failed to find any one piece of the brain that generates consciousness.
Local differences in brain function, however, did predict the return of specific functions. In other words, the activity in the visual cortex predicted the return of vision, while activity in the language cortex predicted the return of language. Therefore, the PET scanning was able to demonstrate not only overall brain activity, but the significance of activity in specific parts of the brain. This helps confirm the lack of a specific part of the brain needed for consciousness, because this study should have been able to show it.
All of this is interesting, but the clinical goal is to determine if such technology can predict overall patient outcome. This study delivered there as well:
Overall, the cerebral metabolic rate accounted for the current level, or imminent return, of awareness in 94% of the patient population, suggesting a global energetic threshold effect, associated with the reemergence of consciousness after brain injury.
PET scan activity specifically predicted the outcome (recovery to consciousness) in 88% of subjects.
Utility
Predicting who is likely to recover from head trauma to the point that they are conscious and able to have some quality of life is extremely useful to family members tasked with making decisions about care.
Patients who are likely to recover based on this type of PET data might benefit from more aggressive care, while patients who have little or no potential to recover can be treated to maximize comfort.
It may seem like it is asking a lot of a diagnostic test to determine the overall care of a patient, but right now those decisions are still being made, just with greater uncertainty as we generally base such decisions on clinical assessment and anatomical imaging. PET scanning, according to this study which also builds upon previous studies, adds another piece of information that can help us make better assessments and predictions.
The fact that this study was able to quantify PET metabolism and consciousness is also extremely helpful. Knowing that there is a threshold, 42%, that is necessary for consciousness is especially useful.
Clearly more research will be necessary to confirm these results and add more details. I would like to see a similar study in patients suffering from other causes of coma, such as diffuse anoxia. The more information we have about PET scanning results and long term outcomes the better.
Families caring for loved-ones in a coma are in a very difficult position. They don’t want to give up if there is hope, but they also don’t want to condemn their loved-one to an existence they may not have wanted if there is no hope. Uncertainty is agonizing, and anything that can reduce uncertainty is extremely useful.